~ Inspectorate of Health Investigating.~
PHILIPSBURG:--- A 36-year-old woman lost her life during the early afternoon on Tuesday at the St. Maarten Medical Center (SMMC) after reportedly having an abdominal myomectomy (major surgery to remove fibroids.) The operation was conducted by local gynecologist Dr. Randal Friday.
SMN News learned that the surgery went well but after she was taken to the ward it was discovered that she was motionless sometime after 2:30 pm it is reported that the patient died of pulmonary embolism (huge blood clot in the lungs.) Further explained that based on what they know the patient was healthy and had no known medical condition.
Several persons in the community also expressed shock at well known young woman's passing saying that she seemed healthy.
SMN News further understands that the Inspectorate of Health Dr. Earl Best has been informed of the death which is now under investigation. It should also be noted that Dr. Best and Dr. Friday have a strained relationship since the Inspector General did everything within his power to block Dr. Friday from practicing medicine on St. Maarten while allowing those he favors to begin working without proper screening. Concerns are already being raised about Dr. Best conducting an impartial investigation.
Dr. Randal Friday has been practicing medicine on St. Maarten for the past 12 years and this is the first time one of his patients lost their lives.
Efforts made to reach Dr. Randal Friday for a comment proved futile as he could not be reached by phone.
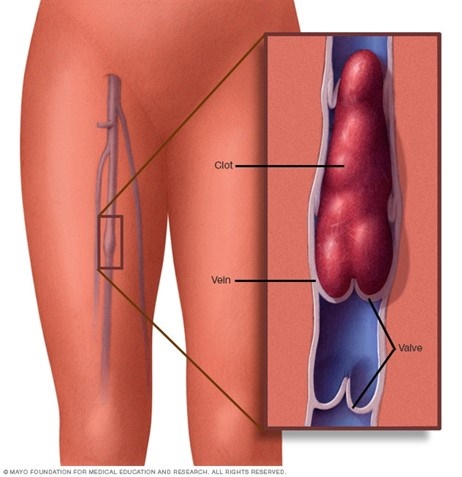
Below is information relating to Pulmonary embolism taken by MAYO Clinic.
Pulmonary embolism occurs when a clump of material, most often a blood clot, gets wedged into an artery in your lungs. These blood clots most commonly come from the deep veins of your legs a condition known as deep vein thrombosis (DVT).
In many cases, multiple clots are involved in pulmonary embolism. The portions of the lung served by each blocked artery are robbed of blood and may die. This is known as pulmonary infarction. This makes it more difficult for your lungs to provide oxygen to the rest of your body.
Occasionally, blockages in the blood vessels are caused by substances other than blood clots, such as:
- Fat from the marrow of a broken long bone
- Part of a tumor
- Air bubbles
Risk factors
Pulmonary embolism occurs when a clump of material, most often a blood clot, gets wedged into an artery in your lungs. These blood clots most commonly come from the deep veins of your legs a condition known as deep vein thrombosis (DVT).
In many cases, multiple clots are involved in pulmonary embolism. The portions of the lung served by each blocked artery are robbed of blood and may die. This is known as pulmonary infarction. This makes it more difficult for your lungs to provide oxygen to the rest of your body.
Occasionally, blockages in the blood vessels are caused by substances other than blood clots, such as:
- Fat from the marrow of a broken long bone
- Part of a tumor
- Air bubbles
Risk factors
Blood clot in leg vein open pop-up dialog box
Although anyone can develop blood clots and subsequent pulmonary embolism, certain factors can increase your risk.
Medical conditions and treatments
You're at higher risk if you or any of your family members have had venous blood clots or pulmonary embolism in the past.
In addition, some medical conditions and treatments put you at risk, such as:
- Heart disease. Cardiovascular disease, specifically heart failure, makes clot formation more likely.
- Certain cancers — especially brain, ovary, pancreas, colon, stomach, lung, and kidney cancers, and cancers that have spread — can increase the risk of blood clots, and chemotherapy further increases the risk. Women with a personal or family history of breast cancer who are taking tamoxifen or raloxifene also are at higher risk of blood clots.
- Surgery is one of the leading causes of problem blood clots. For this reason, medication to prevent clots may be given before and after major surgery, such as joint replacement.
- Disorders that affect clotting. Some inherited disorders affect the blood, making it more prone to clot. Other medical disorders such as kidney disease can also increase your risk of blood clots.
- Coronavirus disease 2019 (COVID-19). People who have severe symptoms of COVID-19 have an increased risk of pulmonary embolism.
Prolonged immobility
Blood clots are more likely to form during periods of inactivity, such as:
- Bed rest. Being confined to bed for an extended period after surgery, a heart attack, leg fracture, trauma or any serious illness makes you more vulnerable to blood clots. When the lower extremities are horizontal for long periods, the flow of venous blood slows and blood can pool in the legs, sometimes resulting in blood clots.
- Long trips. Sitting in a cramped position during lengthy plane or car trips slows blood flow in the legs, which contributes to the formation of clots.
Other risk factors
- For reasons that aren't well understood, tobacco use predisposes some people to blood clot formation, especially when combined with other risk factors.
- Being overweight. Excess weight increases the risk of blood clots — particularly in people with other risk factors.
- Supplemental estrogen. The estrogen in birth control pills and in hormone replacement therapy can increase clotting factors in your blood, especially if you smoke or are overweight.
- The weight of the baby pressing on veins in the pelvis can slow blood return from the legs. Clots are more likely to form when blood slows or pools.
Complications
Pulmonary embolism can be life-threatening. About one-third of people with undiagnosed and untreated pulmonary embolism don't survive. When the condition is diagnosed and treated promptly, however, that number drops dramatically.
Pulmonary embolism can also lead to pulmonary hypertension, a condition in which the blood pressure in your lungs and in the right side of the heart is too high. When you have obstructions in the arteries inside your lungs, your heart must work harder to push blood through those vessels, which increases blood pressure and eventually weakens your heart.
In rare cases, small emboli occur frequently and develop over time, resulting in chronic pulmonary hypertension, also known as chronic thromboembolic pulmonary hypertension.
Prevention
Preventing clots in the deep veins in your legs (deep vein thrombosis) will help prevent pulmonary embolism. For this reason, most hospitals are aggressive about taking measures to prevent blood clots, including:
- Blood thinners (anticoagulants). These medications are often given to people at risk of clots before and after an operation — as well as to people admitted to the hospital with medical conditions, such as heart attack, stroke, or complications of cancer.
- Compression stockings. Compression stockings steadily squeeze your legs, helping your veins and leg muscles move blood more efficiently. They offer a safe, simple, and inexpensive way to keep blood from stagnating during and after general surgery.
- Leg elevation. Elevating your legs when possible and during the night also can be very effective. Raise the bottom of your bed 4 to 6 inches (10 to 15 cm) with blocks or books.
- Physical activity. Moving as soon as possible after surgery can help prevent pulmonary embolism and hasten recovery overall. This is one of the main reasons your nurse may push you to get up, even on your day of surgery, and walk despite the pain at the site of your surgical incision.
- Pneumatic compression. This treatment uses thigh-high or calf-high cuffs that automatically inflate with air and deflate every few minutes to massage and squeeze the veins in your legs and improve blood flow.
Prevention while traveling
The risk of blood clots developing while traveling is low, but increases as long-haul travel increases. If you have risk factors for blood clots and you're concerned about travel, talk with your doctor.
Your doctor might suggest the following to help prevent blood clots during travel:
- Drink plenty of fluids. Water is the best liquid for preventing dehydration, which can contribute to the development of blood clots. Avoid alcohol, which contributes to fluid loss.
- Take a break from sitting. Move around the airplane cabin once an hour or so. If you're driving, stop every so often and walk around the car a couple of times. Do a few deep knee bends.
- Fidget in your seat. Flex your ankles every 15 to 30 minutes.
- Wear support stockings. Your doctor may recommend these to help promote circulation and fluid movement in your legs. Compression stockings are available in a range of stylish colors and textures. There are even devices, called stocking butlers, to help you put on the stockings.
The Mayo Clinic experience and patient stories
Our patients tell us that the quality of their interactions, our attention to detail, and the efficiency of their visits mean health care like they've never experienced. See the stories of satisfied Mayo Clinic patients.
Blood clot in leg vein open pop-up dialog box
Although anyone can develop blood clots and subsequent pulmonary embolism, certain factors can increase your risk.
Medical conditions and treatments
You're at higher risk if you or any of your family members have had venous blood clots or pulmonary embolism in the past.
In addition, some medical conditions and treatments put you at risk, such as:
- Heart disease.Cardiovascular disease, specifically heart failure, makes clot formation more likely.
- Certain cancers — especially brain, ovary, pancreas, colon, stomach, lung, and kidney cancers, and cancers that have spread — can increase the risk of blood clots, and chemotherapy further increases the risk. Women with a personal or family history of breast cancer who are taking tamoxifen or raloxifene also are at higher risk of blood clots.
- Surgery is one of the leading causes of problem blood clots. For this reason, medication to prevent clots may be given before and after major surgery, such as joint replacement.
- Disorders that affect clotting. Some inherited disorders affect blood, making it more prone to clot. Other medical disorders such as kidney disease can also increase your risk of blood clots.
- Coronavirus disease 2019 (COVID-19). People who have severe symptoms of COVID-19 have an increased risk of pulmonary embolism.
Prolonged immobility
Blood clots are more likely to form during periods of inactivity, such as:
- Bed rest. Being confined to bed for an extended period after surgery, a heart attack, leg fracture, trauma or any serious illness makes you more vulnerable to blood clots. When the lower extremities are horizontal for long periods, the flow of venous blood slows and blood can pool in the legs, sometimes resulting in blood clots.
- Long trips. Sitting in a cramped position during lengthy plane or car trips slows blood flow in the legs, which contributes to the formation of clots.
Other risk factors
- For reasons that aren't well understood, tobacco use predisposes some people to blood clot formation, especially when combined with other risk factors.
- Being overweight. Excess weight increases the risk of blood clots — particularly in people with other risk factors.
- Supplemental estrogen. The estrogen in birth control pills and in hormone replacement therapy can increase clotting factors in your blood, especially if you smoke or are overweight.
- The weight of the baby pressing on veins in the pelvis can slow blood return from the legs. Clots are more likely to form when blood slows or pools.
Complications
Pulmonary embolism can be life-threatening. About one-third of people with undiagnosed and untreated pulmonary embolism don't survive. When the condition is diagnosed and treated promptly, however, that number drops dramatically.
Pulmonary embolism can also lead to pulmonary hypertension, a condition in which the blood pressure in your lungs and in the right side of the heart is too high. When you have obstructions in the arteries inside your lungs, your heart must work harder to push blood through those vessels, which increases blood pressure and eventually weakens your heart.
In rare cases, small emboli occur frequently and develop over time, resulting in chronic pulmonary hypertension, also known as chronic thromboembolic pulmonary hypertension.
Prevention
Preventing clots in the deep veins in your legs (deep vein thrombosis) will help prevent pulmonary embolism. For this reason, most hospitals are aggressive about taking measures to prevent blood clots, including:
- Blood thinners (anticoagulants). These medications are often given to people at risk of clots before and after an operation — as well as to people admitted to the hospital with medical conditions, such as heart attack, stroke or complications of cancer.
- Compression stockings. Compression stockings steadily squeeze your legs, helping your veins and leg muscles move blood more efficiently. They offer a safe, simple, and inexpensive way to keep blood from stagnating during and after general surgery.
- Leg elevation. Elevating your legs when possible and during the night also can be very effective. Raise the bottom of your bed 4 to 6 inches (10 to 15 cm) with blocks or books.
- Physical activity. Moving as soon as possible after surgery can help prevent pulmonary embolism and hasten recovery overall. This is one of the main reasons your nurse may push you to get up, even on your day of surgery, and walk despite pain at the site of your surgical incision.
- Pneumatic compression. This treatment uses thigh-high or calf-high cuffs that automatically inflate with air and deflate every few minutes to massage and squeeze the veins in your legs and improve blood flow.
Prevention while traveling
The risk of blood clots developing while traveling is low, but increases as long-haul travel increases. If you have risk factors for blood clots and you're concerned about travel, talk with your doctor.
Your doctor might suggest the following to help prevent blood clots during travel:
- Drink plenty of fluids. Water is the best liquid for preventing dehydration, which can contribute to the development of blood clots. Avoid alcohol, which contributes to fluid loss.
- Take a break from sitting. Move around the airplane cabin once an hour or so. If you're driving, stop every so often and walk around the car a couple of times. Do a few deep knee bends.
- Fidget in your seat. Flex your ankles every 15 to 30 minutes.
- Wear support stockings. Your doctor may recommend these to help promote circulation and fluid movement in your legs. Compression stockings are available in a range of stylish colors and textures. There are even devices, called stocking butlers, to help you put on the stockings.










